A case of 60year old female
Name: J. Akash
31/12/2022
Roll no. 53
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
Following is the view of my case :
patient complaining of fever since 4days
decreased apetite since 4days
difficulty in micturition since 4days
patient was apparently asymptomatic 10years back
then she had H/O bleeding from nipples following diagnosed to have ?fibroadenoma, surgery was done and removed,post op uneventful
5years back patient had swelling at sacral area progressively increased in size, surgical removal was done,post op uneventful
2yeara back patient developed tingling and numbness of B/L upperlimbs and lowerlimbs and was investigated and used medications and was subsided
weakness of upperlimbs and lowerlimbs gradually progressive
1year and 7months back patinet was unable to walk and difficulty in grip,used to walk with support for 4months later weakness progressed and was unable to walk
7months back patient developed pedal edema, burning sensation of feet, investigated to jave compressive myelopathy with spastic qaudriparesis
planned for cervical laminnectomy
1and half month back surgery was done
post surgery patient had difficulty in moving Rt upperlimb, slowly recovered
burning, tingling sensation reduced,pain reduced
tone slightly improved, decreased bowel and bladder movements
4days back patient developed fever highgrade intermittent
No H/O cough,cold, burning micturition , sore throat
H/o abdominal distension,blanching,retrosternal burning sensation
since 4days difficulty in passing urine, decreased urination , unable to pass urine without strain
No H/O hesitancy, urgency, incontinence, increased frequency
voiding of urine and sensations are normal
PAST HISTORY:
Not a k/c/o DM,HTN,TB, EPILEPSY,ASTHMA,CAD
FAMILY HISTORY: insignificant
GENERAL EXAMINATION
pt conscious, coherent, co-operative well orientated to time ,place, person
no signs of pallor, icterus, clubbing,cyanosis,edema,lymphadenopathy
CVS- S1S2+,no thrills and murmurs
RS-trachea,BAE+,NVBS
ABDOMEN:soft,nontender,no palpable mass,liver and spleen not palpable
CNS: pt conscious
speech-normal
no meaningeal signs
INVESTIGATIONS:
Neck Xray C spine
Chest Xray:
USG abdomen
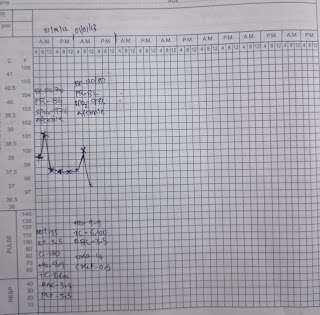
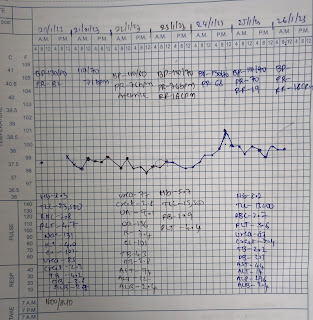
investigation chart:
Diagnosis:
Pyrexia under evaluation ?UTI
with post cervical laminnectomy
with hyponatremia under evaluation
with hypokalemia under evaluation
Treatment Given
IVF NS @100ml /hr
1amp KCL +500ml NS
Inj.neomol 1gm/IV
31/12/2022
UNIT 5
DR HIMAJA, PGY1
DR PAVANI, PGY2
DR SAI CHARAN, PGY3
DR ABHINAYA, SR
DR AKASH, INTERN
DR HYNDAVI, INTERN
AMC, DAY 1
AGE : 60Y GENDER :F
S:
No fever spikes
stools passed
O:
pt conscious, coherent, co-operative
Bp-120/70mmhg
PR-82bpm
Temp-98°FF
GRBS-187 mg/dl
SPO2-97%
CNS-HMF intact
memory -normal
Tone : RT LT
UL N. decreased
LL N. decreased
REFLEXES: B. T. S. K. A. Plantar
RT. + + ++ . ++ + + extension
LT. - - - ++ + + extension
power LT RT
UL. 5/5. 2/5
LL. 5/5. 4/5
A:
pyrexia secondary to ?UTI
with post laminnectomy done(1and half month back)
with hyponatremia (resolved)
with hypokalemia 2° to ? renal loss
P:
IVF NS @100ML/HR
inj.neomol iv/sos
(D1 )Tab nitrofurantoin 100mg po/bd
Syp. POTCHLOR 15ml/po/Tid
monitor vitals
01/01/23
UNIT 5
DR HIMAJA, PGY1
DR PAVANI, PGY2
DR SAI CHARAN, PGY3
DR ABHINAYA, SR
DR AKASH, INTERN
DR HYNDAVI, INTERN
AMC, DAY 2
AGE : 60Y GENDER :F
S:
No fever spikes
stools not passed
no headache
O:
pt conscious, coherent, co-operative
Bp-120/80mmhg
PR-82bpm
Temp-98°FF
GRBS-104 mg/dl
SPO2-97%
CNS-HMF intact
memory -normal
Tone : RT LT
UL N. decreased
LL N. decreased
REFLEXES: B. T. S. K. A. Plantar
RT. + + ++ . ++ + + extension
LT. - - - ++ + + extension
power LT RT
UL. 5/5. 2/5
LL. 5/5. 4/5
A:
pyrexia secondary to ?UTI
with post laminnectomy done(1and half month back)
with hyponatremia (resolved)
with hypokalemia 2° to ? renal loss
P:
IVF NS @100ML/HR
inj.neomol iv/sos
(D2 )Tab nitrofurantoin 100mg po/bd
Syp. POTCHLOR 15ml/po/Tid
monitor vitals






Comments
Post a Comment