INTERNSHIP ASSESSMENT
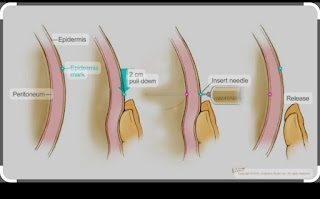
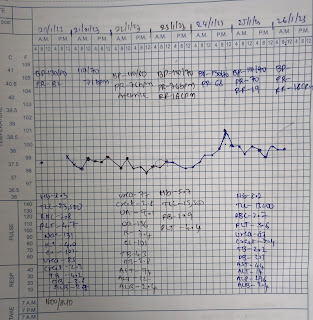
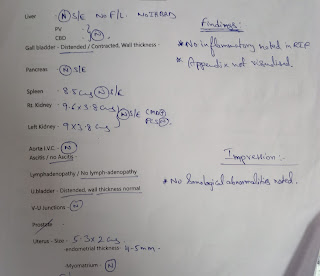
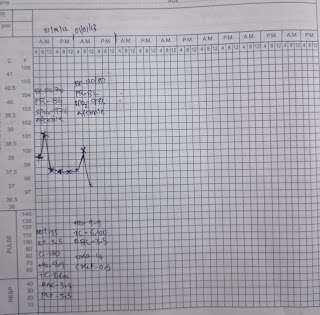
NAME: J. AKASH R. NO -53 ADM NO:176208 I HAVE BEEN POSTED IN GENERAL MEDICINE FROM 12/12/2022 TO 11/02/2023 IN THIS BLOG I'M SHARING MY INTERSHIP WORKING EXPERIENCE PSYCHIATRY DUTIES FIRST 15 DAYS 12/12/2022 TO 26/12/2022 I HAVE BEEN POSTED HERE MY LEARNING POINTS IN PSYCHIATRY POSTING: LEART HOW TO TAKE HISTORY FOR PSYCHIATRY PATIENTS CASES I HAVE SEEN ARE 1.ALCOHOL DEPENDENCE SYNDROME 2.ADJUSTMENT DISORDERS 3..TOBACCO DEPENDENCE SYNDROME 4.SCHIZOPHRENIA 5. OBSESSIVE COMPULSION DISORDER learnt how to manage patients in de-addiction centre checking vitals for patients in op Monitored a case of 55year old male patient with alcohol dependence syndrome. assisted in the management of this patient with the help of Dr nirupama and Dr spandana UNIT DUTIES FROM 27/12/2022 TO 26/01/2023 i was posted in unit for 1month and my pgs were Dr Himaja ,Dr Deepika, Dr Vinay sir for first 1week For remaining days my pgs were Dr Himaja , Dr pavani...