Compressive myelopathy
J. Akash
4th year
This is an online Elog book to discuss our patient deidentified health data shared after taking his/ her guardians sign informed consent
Here we discuss our individual patient problems through series of inputs from available Global online community of experts with n aim to solve those patient clinical problem with collect6current best evidence based input
This Elog also reflects my patient centered online learning portfolio.
Your valuable inputs on comment box is welcome
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competancy in reading and comprehending clinical data including history, clinical finding, investigations and come up with a diagnosis and treatment plan
A 65 year old male patient, farmer by occupation, resident of suryapet has come to the casualty with the chief complaints of
1) Generalised body weakness since 10 days
HOPI
The patient was apparently asymptotic 2 months back
He developed burning micturition one day after which when he was taken to local hospital, found out to be with Kidney problem AKI? He was given oral medicines for 1 week and was sent to home
The same complaint started again after 11/2 month.This time he was given IV medications and sent home after 4 days.
10 days back, he started having generalised weakness which was gradual in onset associated with generalised pain which was of prickling type, neck pain which exacerbated when he tried to get up from supine position.
He also complained of tingling sensation of soles and left wrist pain which was due to a trauma caused by pull.
PAST HISTORY
He had a bee bite 30 years back. Treated with medications
He also had thorn prick 10 days back following which his lower limbs had pigmentation.
PERSONAL HISTORY
Diet- mixed(vegetarian since 2 months)
Appetite- normal
Sleep- adequate
Bowel and bladder movements- regular
Sleep- adequate
Addictions- chutta(2-3 months back) occasional
Occasional drink( once per month)
FAMILY HISTORY
Not significant
GENERAL EXAMINATION
The patient was coherent conscious cooperative well oriented to time place and person
He was poorly built and nourished with muscle wasting
Right foot
Right hand
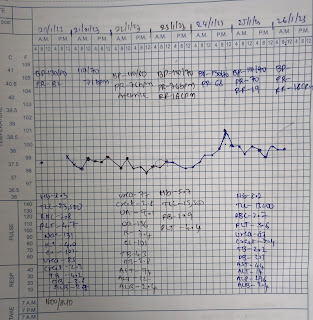
Vitals
Temp - afebrile
BP - 120/80 mmhg
PR - 88 bpm
RR - 18 cpm
SpO2 - 99 at RA
CVS - S1 S2 heard
RS - BAE present, NVBS heard
Per Abdomen- soft, non tender
CNS -
GCS - 15/15
Patient is conscious and alert
Speech is normal
Neck stiffness is present with painful movement of head and raising both upper limbs
Cranial nerves - normal
Sensory system - decreased on right upper limb from C5 to C7 ( shoulder upto palm )
Motor system - Tone normal
Reflexes
Right Left
Biceps Couldn't elicit 3+
Triceps 2+ 3+
Supinator - 1+
Knee 2+ 2+
Ankle - -
Plantar Withdrawal
Muscles power:
Right Left
Upper limb
Elbow - Flexor 5/5 5/5
- extensor 5/5 5/5
Wrist - Flexor 5/5 5/5
- extensor 5/5 5/5
Hand grip 4/5 4/5
Lower limb
SLRT 70⁰ 40⁰
Hip - Flexors 5/5 5/5
- extensors 5/5 5/5
Knee - Flexors 5/5 5/5
- Extensors 5/5 5/5
Ankle - DF 4/5 4/5
- PF 4/5 4/5
EHL 3/5 3/5
FHL 3/5 3/5
Sensation ++ ++
Investigations:
Hemogram
Hb - 9.9
TLC - 14000
RBC - 3.94
Platelet count - 6 lakh
PCV - 31.2
CUE
Albumin- trace
Sugar - nil
Pus cells - 2 - 3
Epithelial cells - 2- 3
Red cells - nil
LFT
TB - 1.7
DB - 0.5
AST - 36
ALT - 49
ALP - 582
TP - 7.6
Albumin - 2.4
RBS - 80
RFT
Urea - 168
Creatinine - 3.5
Sr. Na - 133
Sr. K - 6
Sr. Cl - 90
Serology - negative
Provisional diagnosis:
Compressive myelopathy secondary to prevertebral access/ soft tissue D1 - D3 ? Space occupying lesion D11 - L1 with mild C5 - C6 cord compression









Comments
Post a Comment